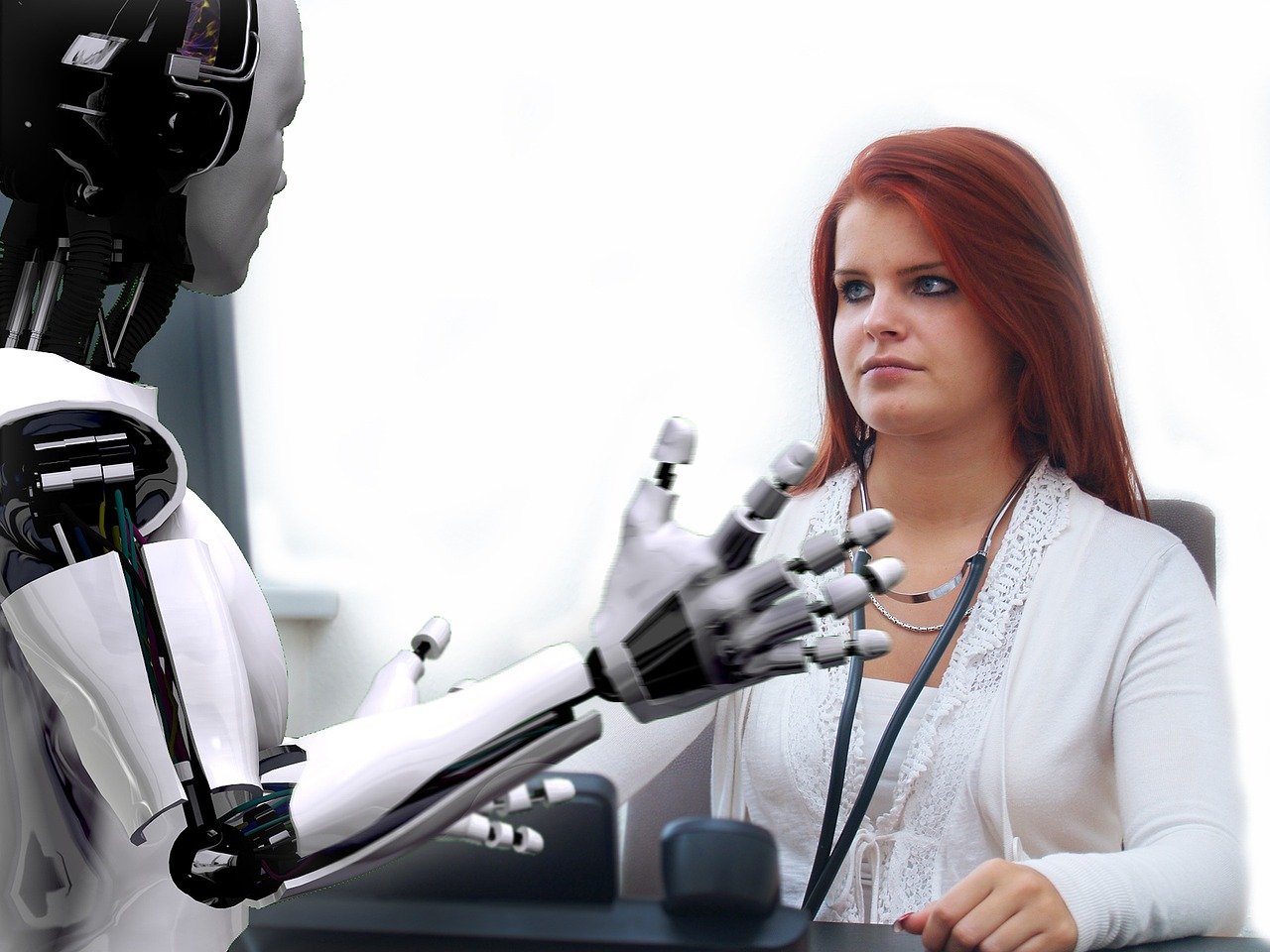
The Effects of Modern Technology on People’s Health
The development of technology lies at the core of human progress, and it is a fact that simply can’t be denied. The areas of life where technological growth has yielded the best results are diverse and encompass anything from production and communication to health and entertainment. The fact that technology […]